Haikara Health
Digitizing the referral of pregnant women in Kenya
Haikara Health is a digital platform for the onboarding and referral of pregnant women between medical facilities. The goal of the project, done in collaboration with Makerspace Nairobi and Aalto Global Impact, was to help facilitate a more reliable and efficient maternal healthcare process in developing regions for pregnant women, healthcare providers, and systemic agents. The project is especially dear to me, not only for the friendships that resulted from it, but also because I think it provides a good case for how digital technologies can be levered to genuinely improve lives by addressing elemental concerns. On the level of technical skills, the project contributed heavily to my professional development since it allowed me to experience a rigid and consequential application of human centered design methodology, including multi-methodical ethnographic research. I also developed a simple but functional full-stack application as a proof of concept for our solution, gaining a solid understanding of the basics of web development in the process. Overall, the project thus helped me to genuinely broaden my previously more business-centered outlook to include ways of problem solving from the fields of design and technology.
Design Research | Service Design | Web Development
TL;DR
I conducted ethnographic research with multiple stakeholders across the Kenyan healthcare system and identified the availability of patient information as a major obstacle in the delivery of healthcare services to pregnant women
I facilitated an onsite co-creation workshop involving nurses and other medical professionals yielding the idea for a digital patient referral platform to ensure continuous information availability and a wholesome patient experience
I steered the communication with key project stakeholders as well as a service design workstream, championing a problem-centric design process
I took sole responsibility for a technology workstream and developed a functional web-prototype for the derived solution (using React, Redux, Express.js, MongoDB, Docker, Nginx, Amazon EC2)
The idea in a nutshell
In Kenya, several thousand women die every year due to complications arising during pregnancy and birth. There are many contributing factors for this, one of them being an inefficient and difficult referral process. This results in failure to provide required medical services or delayed treatment. Another challenge encountered during the project was that medical records were paper based, leading to inaccuracies and a lack of accountability, both of which compromised the overall integrity of the healthcare system.
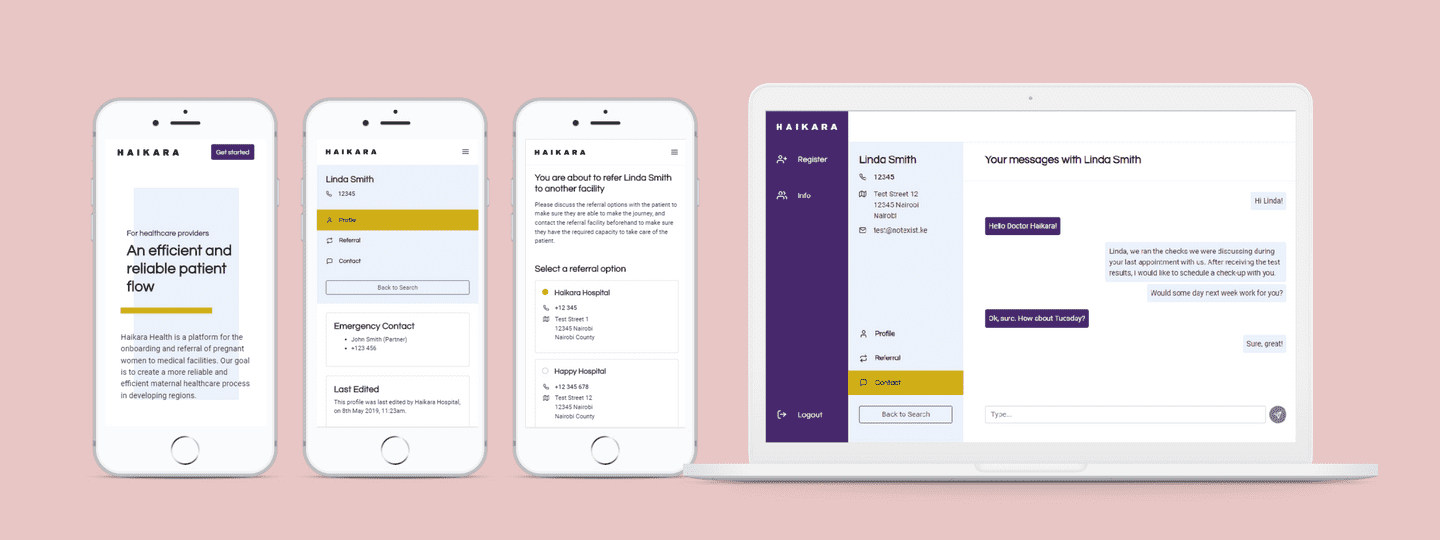
To tackle these issues, we created a centralized solution to improve the overall efficiency of the referral process, enhance the accuracy and reliability of healthcare records and ensure peace of mind for mothers and medical professionals. Haikara Health is a digital platform that enables healthcare facilities to verify and communicate patient information swiftly and confidentially between one another, creating a more efficient and reliable referral process. The platform is also easily accessible by patients, thereby increasing transparency and control over their personal information. The key features of Haikara Health are:
MANAGING PATIENT FLOWS
Haikara Health is designed to digitize the patient onboarding and referral process. The system enables healthcare providers to share patient information, facilitating higher quality patient care across the healthcare delivery system. Haikara Health also relieves medical professionals from administrative efforts during the onboarding of new patients, empowering them to focus their capacities on the mother.
SHARING RELIABLE INFORMATION AT EASE
Haikara Health puts a strong emphasis on patient privacy and information confidentiality. For a healthcare provider to refer a pregnant woman and her information to another facility, she must provide consent. In addition, Haikara Health features an SMS system that is used by pregnant women to communicate with medical professionals and to provide them with all the information they need for a wholesome journey through pregnancy.
PROVIDING HEALTHCARE INSIGHTS
As Haikara Health collects aggregate data, it enables healthcare facilities as well as systemic organizations such as ministries, insurance providers, and NGOs to stay on top of important dynamics within the healthcare system.
Problem identification
To arrive at the concept for Haikara Health, the team went through five months’ worth of research and co-creation - all done in collaboration with the University of Nairobi, local partners such as Kenyatta National Hospital, medical professionals and, of course, expectant mothers themselves. A myriad of solution ideas emerged from these efforts, and after a phase of prototyping and validation, Haikara Health, a solution which empowers both healthcare professionals and expectant mothers, was born.
Our primary goal was to create a concept that would improve lives by increasing efficiencies on a systemic level and that would be scalable across the region and perhaps even across wider Africa, or beyond. As a team, we decided to commit to strictly follow a human centered design process, thus approaching the project with a highly open scope. Consequently, we did not want to prematurely commit to any preconceived ideas for solutions or problems to be focused on. We decided from the outset that decisions would be based on evidence gathered from research, testing and validation, as opposed to assumptions and historical data. Finally, because our project focused on social impact, our guiding goal was to ultimately ensure that whatever we created should first and foremost serve the stakeholders encountered and only to a secondary degree the interests of any institution or organization. We paid, throughout the project, a high level of attention to communicating these choices effectively to all parties involved in the project, so that winning and maintaining the trust of the network of stakeholders in this independent and methodologically rigid approach contributed strongly to my overall learning experience.
Our first step was to build foundational knowledge of the Kenyan healthcare system as well as challenges surrounding maternal health. We then visited Kenya where we collected first-hand insights and information, in cooperation with a team from the University of Nairobi. The research phase of the project was lengthy, but crucial to identifying a real problem that requires solving, based on in-depth desk and ethnographic research. As an outcome, we identified the following main problem areas:
REFERRAL PROCESS
One of the main challenges present at all levels of healthcare and across all stakeholder groups was the referral process. Patients visited facilities based on proximity and availability, crowding units that either are not capable to provide the required services or that are overqualified for it. Medical professionals complained about not being able to track and follow the advancement of a patient throughout the system based on protocols and proper diagnoses.
SHARING PATIENT INFORMATION
Storing and sharing patients’ information was a consistent issue witnessed by different stakeholders. Traditional paper-based reports were predominantly in use although they proved to be ineffective to communicate data to patients, other clinics, and public institutions. This situation motivated private institutions to adopt their own digital solutions. However, the lack of a centralized system did not allow for the transfer of reliable and accurate data pertaining the patient’s clinical history. Patients were often not able to communicate their own information effectively to medical professionals.
TRANSPORTATION
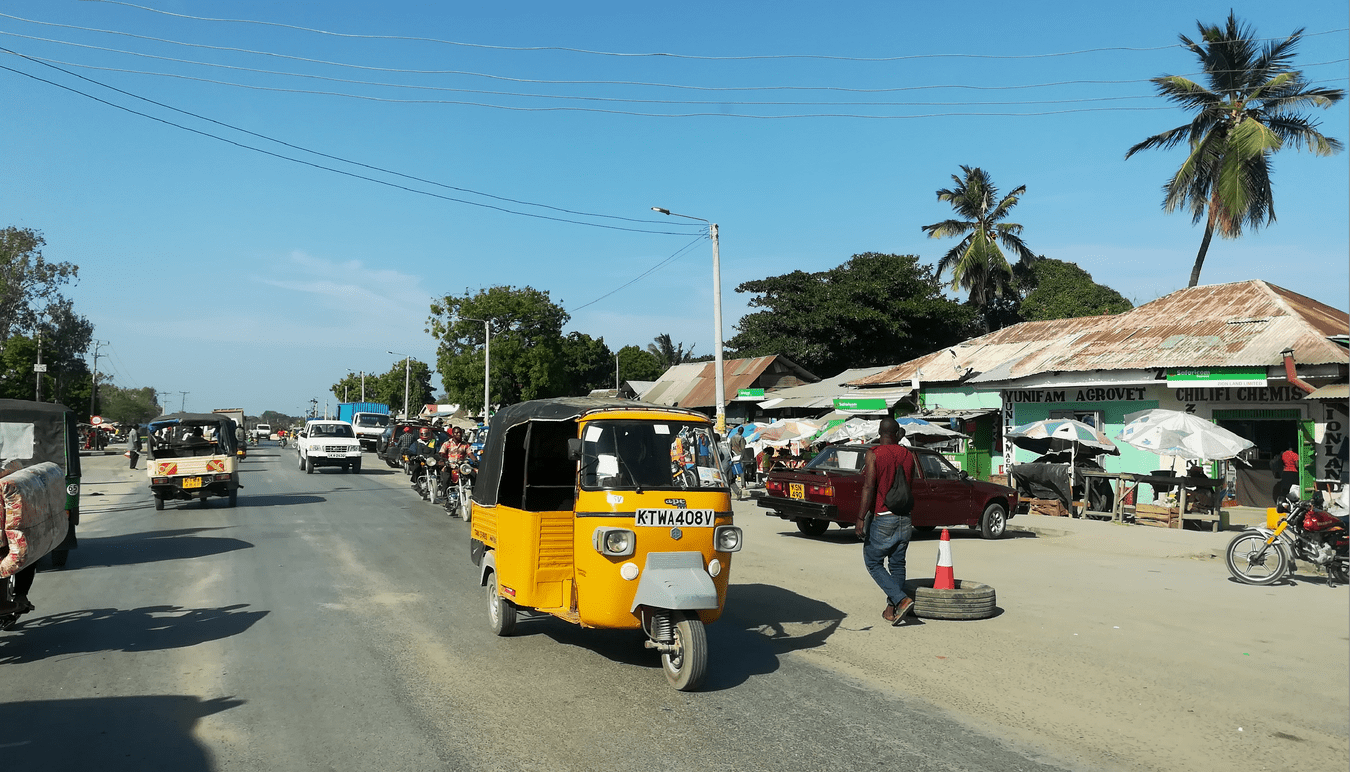
Transportation was a problem identified at community and sub-county level. Patients struggled with finding means to travel from their villages to the closest clinic or hospital. These in turn did not have enough means of transportation available to refer patients to the next level of healthcare. Therefore, patients made use of local transportation such as Tuk-Tuks and motorbikes, even though these presented a risk for the patient’s safety. Nighttime transportation fees were often not affordable for patients, leading to involuntary home deliveries.
FLAWED INCENTIVES
Existing reimbursement policy set flawed incentives for clinics to hold on to patients until delivery and then refer them to higher facilities once complications ensued.


Concept design
After concluding our research, we went through a process of discussing and evaluating the findings with multiple stakeholders, including a co-creation workshop onsite. The outcome was that we identified the way in which patient information was shared across the system as the biggest and most pressing issue in need of fixing. On that basis, we defined several possible design directions relating to problems around the sharing and transfer of patient information. As we progressed and evaluated these, we decided that the main benefit of our solutions should be to enable a more efficient and transparent patient check-in and referral process, allowing clinics to invest more of their scarce resources into patient care. The extended requirement for the final solution was to provide pregnant women with an information service which makes it more who their data is being shared with to build trust, alleviate fears, and provide them with a clearer understanding of the medical process they are going through.
To bring Haikara Health to life and to ensure a holistic, comprehensive result, we developed a service design model to define how the solution should work in practice and how it needs to be presented according to the needs and constraints of its users as well as a functional prototype to establish how such a solution can be technologically implemented and maintained in a scalable way.
Development and prototyping
To define and test the concept, several iterations of a Service Blueprint were developed as a key method to give shape to the idea. Since we had stayed in Kenya only during the research phase, one of the biggest challenges for the project’s development phase was that the team was in a different geographical location than the end users. The team therefore resorted to a plethora of different instruments to test the ideas and get feedback, which included the use of animated videos, surveys, interviews of both end users and experts, and online forum discussions. The Service Blueprint also formed as a contractual document between the different workstreams so that I, being solely responsible for the development of a functional prototype, collaborated with the team on the Blueprint and test planning though I did not participate in the tests themselves.
The prototype was developed to integrate all the findings obtained and demonstrate a possible way to implement the solution. After making a choice regarding the technology basis, the next step in the tech development workstream was to make decisions on the specific technologies and frameworks to be used during the development of the functional prototype. After some research on viable implementation options (catered towards producing a functional prototype in a short amount of time), the decision fell to the favor of the following technological architecture:
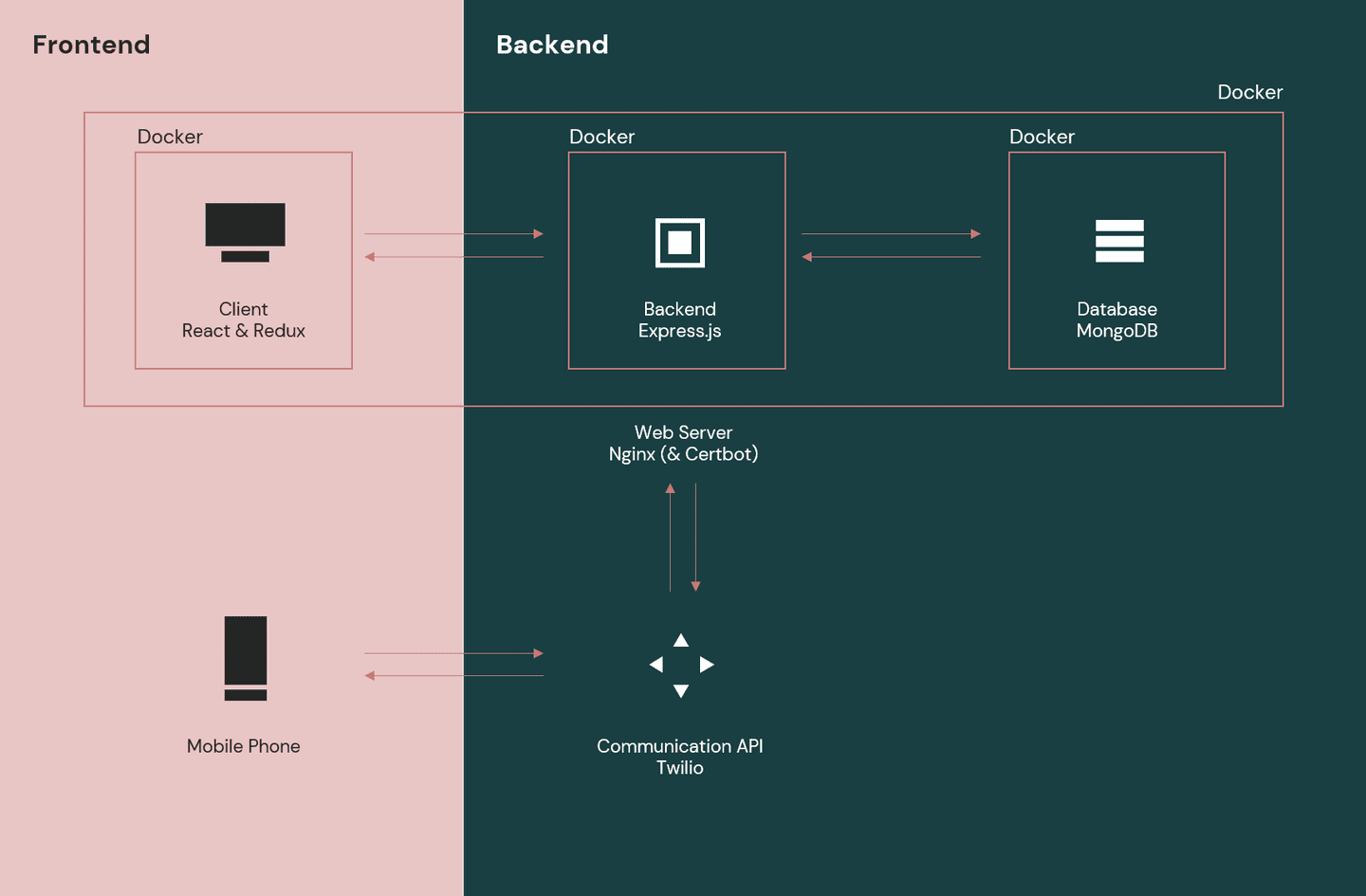
The whole application was hosted on an Amazon EC2. By the end of the project, the web platform (everything contained by the web server) was functional, but not yet connected to the communication API, meaning the application could not yet communicate with patients using SMS. Having had some exposure to frontend but not to backend development beforehand, developing the prototype in a short timespan was quite challenging, but very rewarding, as it provided me with a basic understanding of all key aspects involved in developing and hosting a basic web application.